PTSD Guideline Overview
Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
VA »
Health Care »
PTSD: National Center for PTSD
» Providers
»
PTSD Guideline Overview - Rural Provider PTSD Toolkit
PTSD: National Center for PTSD
PTSD Guideline Overview - Rural Provider PTSD Toolkit
Rural Provider PTSD Toolkit
The Veterans Affairs and Department of Defense Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder was revised in 2017 to provide the latest information and assist clinical decision making in all aspects of a patient-centered care approach.18 A rapidly growing body of research has led to new or refined strategies to manage and treat patients with PTSD. The use of a shared decision making process is encouraged where the patient and provider together review treatment options and compare benefits and harms of each before selecting the option that best meets the patient's needs.
Shared Decision Making
Shared decision making is an approach in which providers and patients communicate together using the best available evidence to make decisions.To learn more, take this PTSD 101 online course: Shared Decision Making for PTSD.
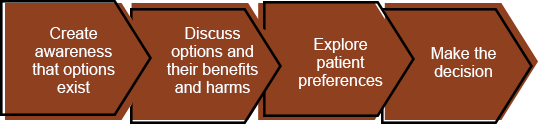
Create awareness that options exist. Discuss options and their benefits and harms. Explore patient preferences. Make the decision.
Diagnosis
An accurate diagnosis and assessment using either a clinical interview or structured diagnostic interview is an essential first step to correctly identify patients with PTSD and ensure they receive appropriate treatment. Brief questionnaires such as the PTSD Checklist (PCL-5) can be used to assess symptom severity and monitor treatment response.PTSD Treatment Guidelines
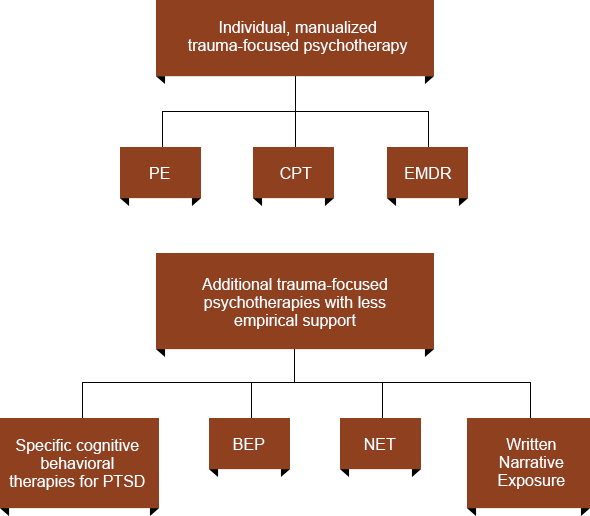
A major change in the 2017 guideline is there is now a recommendation to use specific trauma-focused treatments over medications or other psychotherapies, which are both recommended as second line.The guideline's recommendation to use individual trauma-focused psychotherapy over pharmacotherapy reflects the current state of research into PTSD treatment. Two recent meta-analyses noted that trauma-focused psychotherapies impart greater change with regard to core PTSD symptoms than pharmacotherapies, and that these improvements persist for longer time periods.19, 20 The trauma-focused psychotherapies with the strongest evidence from clinical trials are:
- Prolonged Exposure (PE)
- Cognitive Processing Therapy (CPT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Specific cognitive behavioral therapies (CBTs) for PTSD
- Brief Exposure Therapy (BEP)
- Narrative Exposure Therapy (NET)
- Written Narrative Exposure
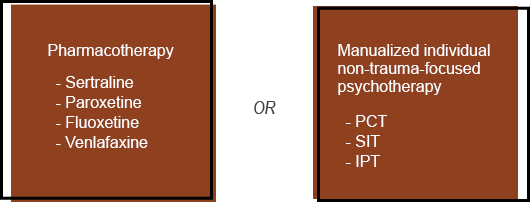
- Stress Inoculation Training (SIT)
- Present-Centered Therapy (PCT)
- Interpersonal Therapy (IPT)
For those patients who choose not to engage in or are unable to access trauma-focused psychotherapy and opt for medication treatment, the use of the specific antidepressants as monotherapy is recommended:
- Sertraline (Zoloft®)
- Paroxetine (Paxil®)
- Fluoxetine (Prozac®)
- Venlafaxine (Effexor®)
First-Line Treatment Recommendations
Second-Line Treatment Recommendations
There is a large group of medications and substances recommended against for PTSD due to low quality of evidence and risk of potential harms. That group includes:
- Atypical antipsychotics
- Benzodiazepines
- Anticonvulsants
- Ketamine
- Hydrocortisone
- D-cycloserine
- Cannabis
Benzodiazepines
- Drowsiness
- Fatigue
- Memory impairment
- Dependence
- Withdrawal symptoms
- Impaired coordination
- Car accidents, falls, fractures
- Worse talk therapy outcomes
- Disinhibition
- Anxiety, irritability, anger
- Negative respiratory outcomes
- Reproductive risk
- All cause + unintentional overdose mortality
Atypical Antipsychotics
- Sedation
- Movement disorders, akathisia
- Anticholinergic effects
- Psychiatric effects
- Apathy, withdrawal
- Orthostatic hypotension
- Metabolic effects
- Weight gain, hyperglycemia, diabetes, dyslipidemia
- Reproductive risk
- Sudden cardiac death, arrhythmia
- Stroke
- Mortality
Despite recommendations against their use in treating PTSD, benzodiazepines and atypical antipsychotics continue to be prescribed in patients with PTSD. In VA, clinicians prescribe benzodiazepines to a third of Veterans with PTSD and do so more often in rural Veterans.23,24 Though prescribing clinicians generally agree with practice guidelines that discourage harmful medication use in PTSD, often they do not taper patients off because tapering is too time-intensive or because the patients appear stable.25 There is also a common dilemma in balancing treatments the patient thinks are useful with science and best practice.
When helping a patient already taking harmful drug combinations, it is important to address tapering in a collaborative way, using shared decision making (discussed above).26
There is another large group of medications where the evidence is insufficient to recommend for or against their use. A significant change in the revised 2017 guideline is seen regarding the use of prazosin. The current recommendation suggests against prazosin for global symptoms of PTSD based on lack of efficacy and insufficient evidence to recommend as mono- or augmentation therapy for nightmares.
Despite considerable interest in alternatives to either psychotherapy or medication for the treatment of PTSD, there is currently insufficient evidence to recommend the majority of somatic therapies or complementary and integrative treatments including any animal-assisted therapy.
There is another large group of medications where the evidence is insufficient to recommend for or against their use. A significant change in the revised 2017 guideline is seen regarding the use of prazosin. The current recommendation suggests against prazosin for global symptoms of PTSD based on lack of efficacy and insufficient evidence to recommend as mono- or augmentation therapy for nightmares.
Despite considerable interest in alternatives to either psychotherapy or medication for the treatment of PTSD, there is currently insufficient evidence to recommend the majority of somatic therapies or complementary and integrative treatments including any animal-assisted therapy.























